Threat AID
Clinical tool for clinicians who encounter a patient at risk of targeted or mass violence
The purpose of the Threat AID tool is to provide clinicians with a systematic approach to evaluation once they have identified a patient at risk of targeted or mass violence.
Expressions of violent ideations and/or leakage (communications indicating violence is being considered or planned) are common reasons patients present to mental health care. They may be referred by a third party explicitly for this reason, or the clinician may be the first to identify the concern. Identifying those at elevated risk is beyond the scope of this tool, which is designed to ensure appropriate steps are followed after risk is identified.
More specific resources for identifying those at risk of targeted or mass violence can be found at the bottom of the page.
HIPAA exceptions and other privacy regulations:
HIPAA is not intended to be a barrier to threat assessment and management.
- If a patient makes a “serious and imminent threat” of violence, PHI can be disclosed that is necessary to prevent or lessen the threat and is made to a person(s) reasonably able to prevent or lessen the threat. (source)
- Furthermore, “HIPAA expressly defers to the professional judgment of health professionals in making determinations about the nature and severity of the threat to health or safety posed by a patient. OCR would not second guess a health professional’s good faith belief that a patient poses a serious and imminent threat.” (source)
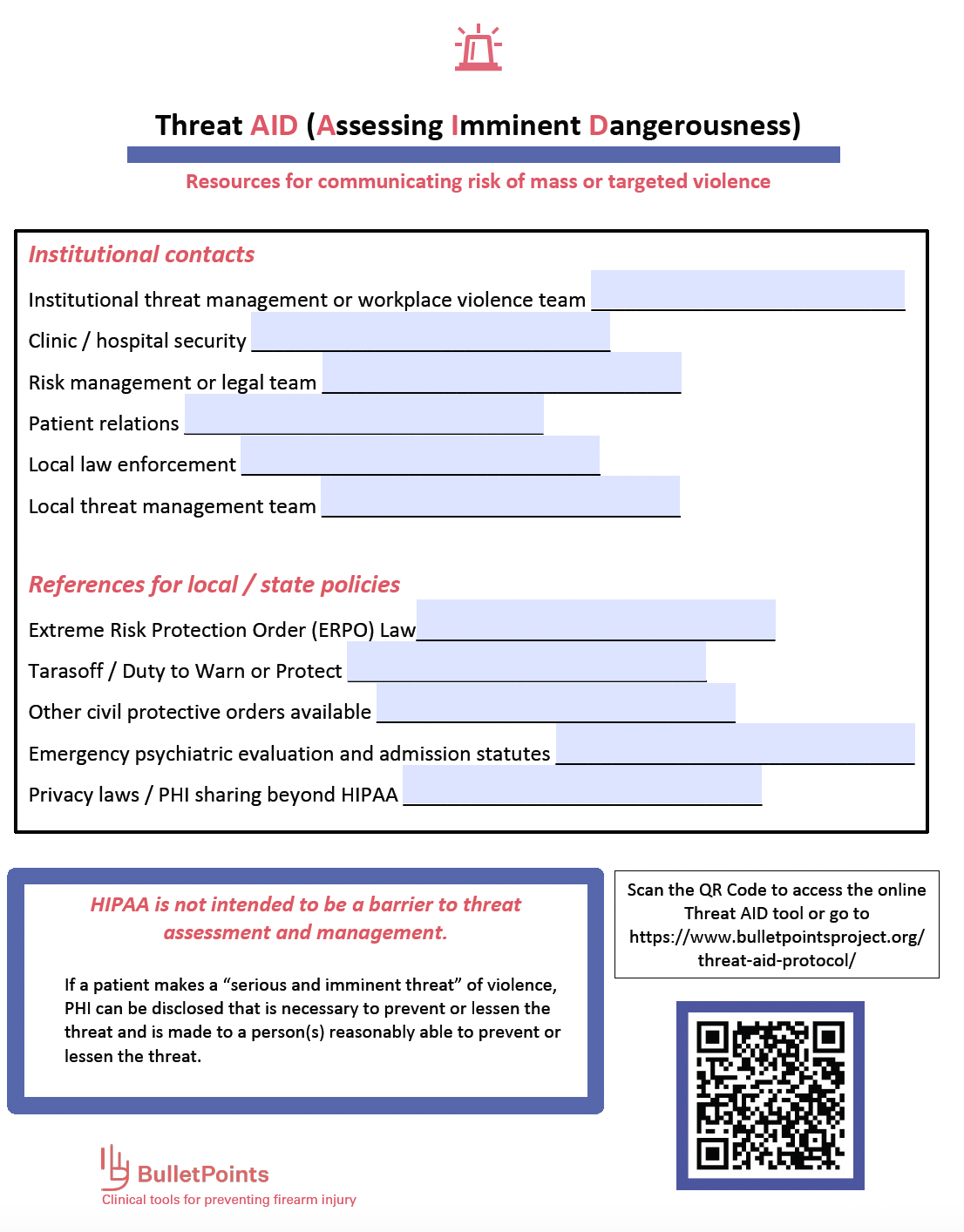
Threat AID Printable Contact Sheet
This section allows your institution or organization to customize this tool with internal and local contacts, resources, laws, and policies relevant to threat management. A copy can be filled in and printed, then posted in workspaces to share information. Whenever possible, include links to reporting systems, points of contacts’ emails, resource hubs, websites, etc.
Click to view steps of the Threat AID tool
- If not recently assessed by psychiatry / available mental health team, involve them as soon as possible
- Screen for suicide risk
There is substantial overlap between mass violence and suicidality, including suicide by third party (e.g. law enforcement, armed on-site security).
- Have a low threshold to hold involuntarily, especially if:
- There are paranoid / delusional / psychotic motivations for threats, especially command hallucinations to act violently or to engage in protective / pre-emptive violence
- Patient has not had previous in-depth psychiatric assessment (beyond what can be done in acute / crisis setting)
- There is co-morbid suicidality
- You need to buy time in a high-risk situation where there may be a benefit to inpatient psychiatric treatment
- Considerations for less restrictive dispositions than inpatient psychiatric hospitalization:
You do not have to hold every time if patient is well known and there is a mitigation plan in place or alternatives more likely to effectively mitigate risk. Examples include:
- Multiple recent admissions with little change with similar presentation
- Good documentation that they are not likely to benefit from inpatient psychiatric intervention (e.g. ASPD, malingering)
- Collaboration with other agencies aware of case (e.g. school, law enforcement, threat management team) on a plan that can mitigate risk in a less restrictive environment
Remember that a psychiatric hold itself is not likely to lead to removal of a person’s access to firearms or prohibit future purchases.
When possible, get in touch with family, school officials, employers and peers. If collateral is not available, document your attempts to get in contact.
Inquire about:
- Concerning statements, messages, or social media posts
- Weapons interest, familiarity, and attempts at acquisition
- Psychiatric history and symptoms
- Past and recent violence, ideation, or leakage
- Personal ideology (e.g. religious extremist, incel, hate group affiliations)
- Recent stressors including relationship or job loss
- Perceived victimization or grudges
- Substance use
- History of stalking or intimate partner / domestic violence
- Relevant internet usage (e.g. ideology-specific chat rooms / message boards, weapons manufacturing or acquisition, previous mass attackers)
- Previous suicide attempts
Each case is an opportunity to build future partnerships with law enforcement for the next case so you have contacts, allies and resources.
- Make sure they are aware of the threat / behaviors of concern
- Present and collect relevant collateral so all parties have all information
- Determine if there are criminal charges being brought / status of investigation / arrest / pending hearing dates
- Collaborate with internal and external authorities for plan to prevent patient from acting during investigation / treatment
- Check firearms and ammunitions purchasing record if possible
- Communicate any statutory duty to warn / protect information, including threats or concern for suicide by cop or other authority
- Discuss petitioning for ERPO and other protective orders where appropriate and available
- Consider other relevant authorities including child protective services, school resources, etc.
Ultimately, threat mitigation is usually an ongoing and iterative process involving multiple disciplines and agencies. It is most likely to be successful when everyone shares information and ideas.
The availability of various types of protective orders including Extreme Risk Protection Orders (aka “red flag laws”) and the requirements of Duty to Warn and Protect laws (aka “Tarasoff statutes”) varies by state; be familiar with the policies / mandates in your area.
- Work with law enforcement on safety protocols and other protective orders as applicable for target(s) identified
- Can include domestic or intimate partner violence, workplace violence, school violence protective orders as appropriate and available
- Fulfill any Duties to Warn or Protect (“Tarasoff” warnings)
- Be aware of statutory duties to warn of protect, which vary by state and action required – map
Many protective orders include orders to relinquish firearms and prohibit future purchasing, in addition to other protections. Extreme Risk Protection Orders are specifically focused on firearm removal and can be applied to a broad range of situations.
- If firearm access or acquisition is a concern, consider an ERPO where available –map
In most states clinicians cannot be petitioner, but can collaborate with family or law enforcement to educate them about need and support them in filing.
- If the patient is a minor, work with family to ensure all firearms out of the home and inaccessible to patient via temporary transfer or safe storage (source)
These steps can be ancillary to arrest or psychiatric holds, as neither will necessarily result in a firearm prohibition
- Inquire about access to and plans to utilize alternative weapons including:
- Explosives
- Vehicles
- Knives / bladed weapons
- Poisons / chemicals
Consultation with a colleague can generate new ideas, help fill any gaps in response, and provide medicolegal backup
- Notify and consult with appropriate people at your institution’s risk management, legal, or security / threat assessment and management departments
- If concerns for internal facility danger, contact facility security
Imagine reading your notes publicly after an adverse outcome and document accordingly!
- Use neutral, objective, patient-centered language
- Use quotations of direct patient language whenever possible
- Document pertinent facts as well as your reasoning on the plan
- Include:
- Access to weapons or intent / ability to acquire
- Collateral sources (or what attempts were made to contact them if none available)
- If psychiatric hold not applied / patient discharged, justification and list of other options leveraged
- Risk and protective factors that can be leveraged later
- Suicide risk assessment
- Potential targets, steps attempted to contact / warn them
- Discharge of statutory duties to warn / protect
- Consultation with colleague, name, and what was discussed
- Law enforcement officer name, agency, and what was discussed
- Other agencies (school, child protective services, e.g.), name and what was discussed
- Action taken to lessen threat to third parties as well as to patient (e.g. protective order, Tarasoff, medication, psychiatric hold, follow-up treatment plan)